TSW Syndrome and Resources for Doctors
ITSAN is a member in good standing of the Coalition of Skin Diseases and an affiliate cited in the Patient Advocate Resource Center of the American Academy of Dermatology. See our About ITSAN tab for more information.
This page is a resource for Healthcare Providers seeking answers from the literature about Topical Steroid Withdrawal Syndrome (TSWS). This information comes directly from the literature via doctors and researchers who have experience with TSWS. Additional commentary and photos with perspective from ITSAN’s worldwide network of TSWS sufferers complete the clinical picture.
Q: What are other names for TSW Syndrome in the literature?
Q: How does TSWS present?
Q: How can TSWS be differentiated from severe Eczema?
Q: How does TSWS present in children?
Q: How is TSWS treated?
Q: What is the time frame for TSWS to resolve?
Q: Are TSWS patients ‘Steroid Phobic’?
Q: What is the prevalence of TSWS?
Q: How can TSWS be prevented?
Q: What are other names for TSW Syndrome in the literature?
At a glance:
Click the term below to link to an example of where each term is used within the literature:
Excerpts from the literature:
Journal of the American Academy of Dermatology, March 2015:
“Nomenclature: Using our a priori definition of TCS withdrawal, the following names listed were used to describe this entity: facial corticosteroid addictive dermatitis, red skin syndrome, topical corticosteroid induced rosacea-like dermatitis, steroid addiction syndrome, steroid withdrawal syndrome, steroid dermatitis, post-laser peel erythema, status cosmeticus, red scrotum syndrome, chronic actinic dermatitis, anal atrophoderma, chronic eczema, corticosteroid addiction, light-sensitive seborrheid, perioral dermatitis, rosacea-like dermatitis, steroid- rosacea, and steroid dermatitis resembling rosacea.” (1)
ITSAN Support Community:
Within the ITSAN Support community, the following terms are used almost exclusively: Topical Steroid Addiction (TSA), Topical Steroid Withdrawal (TSW), and Red Skin Syndrome (RSS). TSW Syndrome can occur when using topical or oral steroids for any purpose, in susceptible individuals. ITSAN has chosen to use TSW Syndrome (TSWS) as an umbrella term to describe the disease until medical consensus is reached concerning naming.
Q: How does TSWS present?
At a glance:
|
|
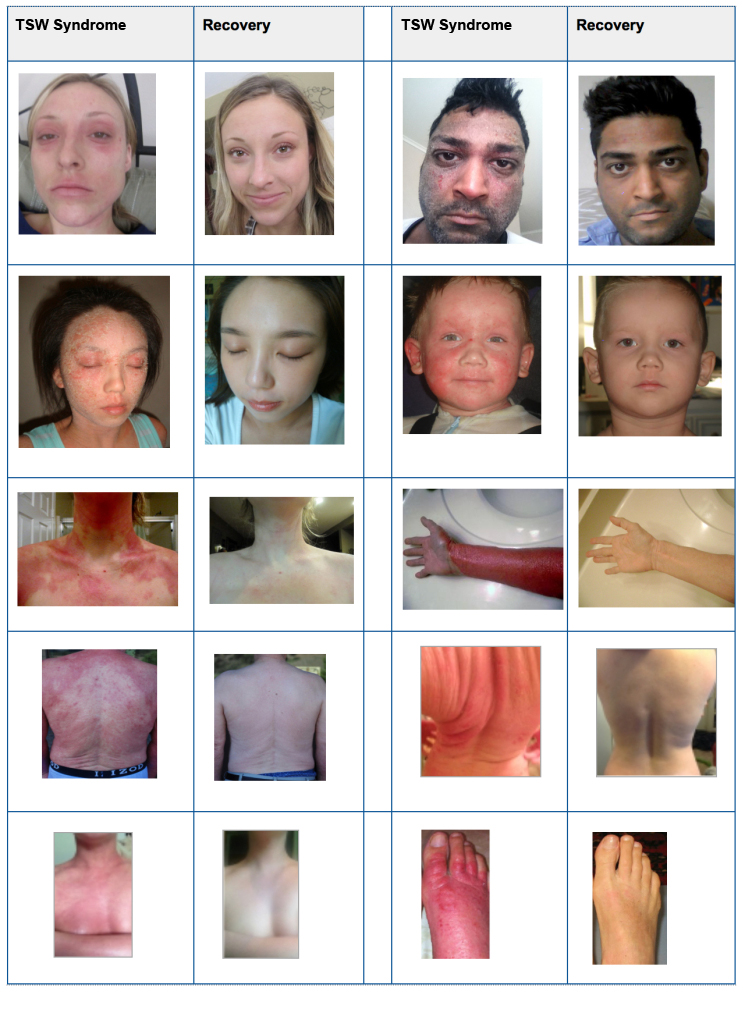
Below are pictures submitted by members of the ITSAN community to illustrate how TSW Syndrome typically presents, and eventually resolves, by total cessation of topical steroids.
Excerpts from the literature:
|
|
|
|
|
|
ITSAN Support Community:
TSWS appears in our members without regard to area treated or topical steroid potency. Some members, especially infants and children, develop TSWS after very short periods, using low potency topical steroids on very small areas of the body. The first symptoms are usually spreading rashes and red, inflamed, itching, burning skin. Doctors have often advised treating more often, on larger areas, with a higher potency topical steroid. This exacerbates the problem as the burning, diffuse rash spreads to other areas of the body.
If topical steroid therapy is withdrawn (even for brief periods between treatments), topical steroid withdrawal symptoms emerge: burning, stinging, oozing, massive flaking, swelling, swollen lymph nodes, elevated IgE levels, etc. As topical steroid withdrawal progresses, the “syndrome” symptoms emerge: insomnia, fatigue, altered thermoregulation, appetite changes, loose skin, hair loss, endocrine symptoms, immunological symptoms, etc.
If steroid therapy is resumed, success is short-lived before leading to the same cycle of escalating symptoms. More aggressive treatment with super high potency topical steroids, oral steroids, or injected steroids lead to severe rebound upon cessation as well as withdrawal symptoms. Please see the “What is TSWS?” tab for a detailed list of TSWS symptoms before and after topical steroid withdrawal.
Q: How can TSWS be differentiated from severe Eczema?
At a glance:
| Eczema | Topical Steroid Withdrawal Syndrome |
|---|---|
| Etiology: Spontaneous. Occasional family history of eczema. | Etiology: History of topical steroid use with progressive exacerbation of original condition |
| Itchy | Burning, stinging, incessant itch |
| Flakey | Constant, profuse shedding of skin flakes (“snowing”) |
| Patches | Diffuse, flushing rashes; erythema; general skin vasodilation; weeping/oozing |
| Patches cycle, resolve, clear, and include periods of remission post treatment with topical steroid | Rebound flares usually occur within days post topical steroid therapy, with increasing severity. Diligent topical steroid therapy becomes less effective over time with little or no period of remission. |
| Symptoms are skin-related: skin discomfort, sleep disruption, and self-consciousness | Symptoms constitute a syndrome in addition to skin issues: enlarged lymph nodes, edema, altered thermoregulation, hair loss, extreme fatigue, appetite changes, hypersensitivity, nerve pain. |
Excerpts from the literature:
|
|
|
ITSAN Support Community:
Eczema and Topical Steroid Withdrawal Syndrome are easier to differentiate if the clinician knows the history of corticosteroid use of the patient, and has close follow-up with the patient between treatments. Unlike eczema, TSWS escalates over time despite aggressive topical steroid therapy. TSWS has a distinctive presentation that is not typical of eczema, especially after ceasing topical steroid therapy. Our community reports that the skin symptoms, as well as the syndrome symptoms, are nothing like the original eczema. Many in our community did not present with eczema in the first place. Some experienced TSWS from topical steroids in cosmetics or skin products, some from being a caregiver and applying topical steroids to another person, while others experienced it without any previous skin condition after receiving oral or injected corticosteroids.
Q: How does TSWS present in children?
At a glance:
- Presentation and treatment is similar to that of adults
- The clinical picture is variable, taking an average of 1 year to clear
- Pediatric community must be alerted to this avoidable and difficult problem
- No large-scale studies have attempted to quantify the incidence of TSWS in children
- Cases of TCS withdrawal in the pediatric population are underreported
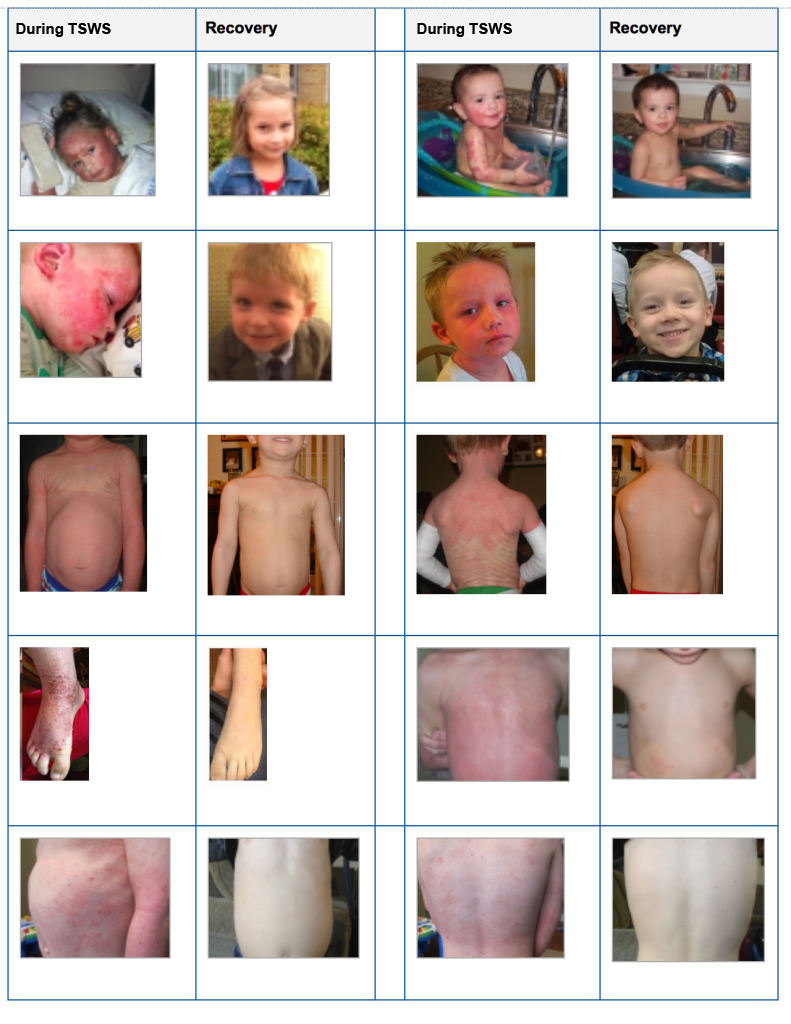
Below are images of children from the ITSAN support group who have recovered after ceasing use of topical steroids:
Excerpts from the literature:
|
|
|
|
|
ITSAN Support Community:
The pediatric population represents a sizable percentage of the ITSAN support group. The symptoms in children mirror the symptoms in adults, and treatment modalities are comparable. Children seem to recover more rapidly than adults — though recovery times vary. Generally speaking, children with TSW have severe withdrawal symptoms in the first 6 months and make significant progress by 12-18 months off topical steroids, with the majority returning to normal life (whether completely symptom free or not) within 24 months. TSW Syndrome is woefully underreported in the pediatric population. Prevalence is not known and is therefore assumed to be rare. However, “rare” must never be confused with “non-existent.” Prevention and/or early recognition is key.
Consider TSW Syndrome for pediatric patients whose mild eczema becomes widespread and aggressive, despite meticulous use of topical steroids, exactly as directed. Reconcile all use of over-the-counter topical corticosteroids, as well as prescriptions written by other specialists: allergists, pediatricians, dermatologists, family doctors, etc. Has the patient also used other forms of corticosteroids, especially concurrently? Side effects, including TSWS, are even more likely with a cumulative steroid load of topical steroids, nasal sprays, metered dose inhalers, nebulizers, and/or oral steroids.
For more insight into TSW Syndrome in children, please see this review: “A systematic review of topical steroid withdrawal in children diagnosed with eczema,” which analyzes data from the blogs of 26 children with TSWS. (16)
Q: How is TSWS treated?
At a glance:
| Symptom | Treatment |
|---|---|
| Topical Steroid Withdrawal Syndrome | Total cessation of topical steroid therapy (no consensus on tapering vs “cold turkey”) |
| Burning | Cold compresses, tepid baths, mineral water sprays (refrigerated), wet wraps |
| Stinging/ Nerve pain | Oral Gabapentin, Pregabalin, pain medications |
| Itching/Pruritus | Oral antihistamines (Diphenhydramine, Hydroxyzine), Doxepin, Topical Pramoxine, dry wraps (gauze, eczema wear, gloves) |
| Oozing/weeping | Burow’s solution (Domeboro), Zinc paste, Viscopaste bandages |
| Infection/Inflammation | Topical/Oral antibiotics, Antivirals, Antifungals – per swab for culture and sensitivity. |
| Insomnia | Sleep aids, relaxation techniques |
| Anxiety/Depression | Anxiety medications/anti-depressants, phone calls, frequent follow-up, emotional support |
| Skin shedding/flaking/peeling | Emollients, dry wraps (gauze, eczema wear, gloves) |
| Rashes/Itching in later stages of TSWS | Narrowband UVB light therapy |
Excerpts from the literature:
|
|
|
|
|
|
|
|
|
ITSAN Support Community:
The vast majority of our members ceased topical steroids “cold turkey.” Our members report that tapering topical steroids (whether by substituting a weaker steroid or using less of often, or both) seemed to prolong the steroid rebound phase. To date, a topical steroid “step down” method without rebound or relapse of symptoms has not been discovered. However, step down therapies may (in theory) be helpful in reducing the systemic symptoms of the syndrome. Successful treatment regimens include ceasing topical/oral/injected corticosteroids, treating symptoms, and monitoring for infection.
Narrowband UVB light therapy can be a helpful option in the later stages of TSWS, when the skin is no longer raw, burning or oozing. UV therapy can cause irritation when used in the early stages, so caution must be used.
Immunosuppressants and immunomodulators have also helped some of our community members lessen the severity of TSWS symptoms. However, these medications are not meant to be used long term. There are side effects and risks that all patients need to be aware of to have proper informed consent. Many in the TSW community also experienced short-lived relief, with return of symptoms and/or new symptoms over time – mirroring their topical steroid withdrawal experience.
Infections reported in support groups are most commonly Staph, MRSA, and Eczema Herpeticum. Skin is open and vulnerable to infection during TSWS, so physician support and close monitoring is imperative. Treatment methods for infection and infection prevention include: swabbing for infection, antibiotics (oral or topical), antivirals, bleach baths, apple cider vinegar baths, saltwater baths, as well as dry wrapping (or with an emollient) in gauze, eczema wear, and gloves. Many of our members also seek out alternatives for infection prevention which include silver sprays, antibacterial essential oil blends, coconut oil, etc. Please see the “Coping with TSWS” tab for tips culminating in a “Survival Guide” for TSWS sufferers from one member to another.
The most important things to remember when treating TSWS topical steroid cessation is imperative, the time frame is protracted, symptoms vary at different stages, and treatment must be tailored to the individual.
Q: What is the time frame for TSWS to resolve?
At a glance:
- Recovery is protracted
- Time required to recover is proportionate to the time topical steroids were used
- Symptoms take many months to several years to resolve
Excerpts from the literature:
|
|
|
|
|
|
ITSAN Support Community:
Within the ITSAN community, recovery time is variable, protracted and measured in months to years. Full recovery from all symptoms takes years for the vast majority. There have been several cases that resolved in 12 months or less, but these are not common within the TSWS community. There seems to be a misunderstanding in the medical community about length of time required to resolve TSW Syndrome; the persistent belief is that the time frame is far too prolonged to be accurate. However, both the literature and reports within the ITSAN support groups reveal that recovery is a lengthy process that is not linear – often described as “two steps forward, one step back.”
The path to recovery is marked by repeated flares and calm periods, with symptoms generally being the most severe during the first year. Flares eventually become few and far between, less severe, and no longer full body. Many report becoming fully clear after TSWS resolves, while some (especially children) report returning to typical eczema-looking patches in conventional places (hands, feet, behind the knees, creases of elbow, etc.). Our members report preferring to treat residual patches without steroids, as opposed to risking relapse of TSWS. Current therapies focus on comfort and infection prevention. More research is needed to discover treatments that could possibly speed up the recovery time frame. Cortisone-free alternatives need to be sought out for these patients who can no longer tolerate topical steroid therapy.
Q: Are TSWS patients ‘Steroid Phobic’?
At a glance:
- Patients who discontinue steroids are not “steroid-phobic,” but are seeking to treat TSW Syndrome in earnest
- Recovery is achieved by discontinuing topical steroids, steroid phobia is a separate issue
- TSWS results from use of topical steroids, not “underuse” or avoidance
Excerpts from the literature:
|
|
ITSAN Support Community:
This is a sensitive topic within the community. Our members have all used topical steroids diligently in the past. However, topical steroid therapy was ineffective and created a new, more severe problem. The term “phobia” denotes extreme or irrational fears. TSWS patients are not abstaining from a treatment based on irrational fears — they are abstaining from a treatment that has caused an iatrogenic condition.
According to a recent poll of the ITSAN Support community, 99.99% of those polled (160 people) used prescription topical steroids, as opposed to strictly over-the-counter. In a subsequent poll, 86% reported developing TSWS while using their medication exactly as their doctor prescribed. This is a patient population who sees their doctors, fills their prescriptions and uses them as directed. This is not a population that is afraid of medical therapies. TSWS is a corticosteroid-induced condition that requires cessation of steroid therapy to treat the condition — this must never be confused for “steroid phobia.”
Q: What is the prevalence of TSWS?
At a glance:
- Prevalence of TSWS is unknown
- TSWS is underreported and not well characterized
- TSWS is more common than realized, but frequently goes unrecognized
Excerpts from the literature:
|
|
|
|
|
ITSAN Support Community:
Members of our community have often expressed that prevalence is underreported. Many have even suggested making themselves or their children case studies, but treating doctors have rarely done so. Because so few pediatric cases exist in the literature, doctors may be hesitant to diagnose this condition in children. This actually perpetuates under-diagnosing and underreporting. Our community represents thousands of people, including children, yet only a few have doctors who recognize TSWS. Accurate diagnosis is key to not only providing care, but precise prevalence data. ITSAN is striving to raise awareness of this often unrecognized disease. In addition, ITSAN is laying the groundwork to organize a patient registry so that prevalence can be more accurately represented. As of now, there is no process for reporting or accessing prevalence data. To best support our patient population, please report any and all cases of TSWS that you diagnose and treat. Please publish case studies. In addition, please contact us at info@ITSAN.org to be placed on our internal physician referral list.
Q: How can TSWS be prevented?
At a glance:
- Physicians must avoid inappropriate prescribing and lax monitoring of refills
- Patients should be counseled regarding the risks, including TCS withdrawal/RSS
- The best time to prevent TSWS is when topical corticosteroids are first prescribed
- Safe and effective long term treatment does not include daily use of TCS
- Perform medication reconciliation — be sure to ask specifically about topical products
- Proper guidance, respectful usage, and close monitoring are key
- Avoid TCS as a first line treatment
Excerpts from the literature:
|
|
|
|
|
|
ITSAN Support Community:
Many feel that their TSWS could have been prevented if: (1) they had been educated about the predisposing factors/risks of TSWS, (2) their topical steroid use had been closely monitored, and (3) steroids had not been prescribed as a “first line” treatment.
Many point out that they were not properly educated on topical steroid use by their healthcare provider – particularly how long is “a long period of time,” how much is “too much” or what constitutes a “large area of the body.” They feel the instructions given by their doctors, such as “use on affected areas,” gave no parameters on how long to treat or how large an area was safe to treat. The “affected area” was often a “large area of the body” and grew larger over time, but this was not usually addressed. In addition, some patients were encouraged to use their prescription “off label.” Assertions of “steroid misuse,” “steroid overuse” or even “steroid underuse” places undue blame on the patient who is actually using exactly as directed by their doctors.
Members report that their physician did not ask about their topical steroid use. Prescriptions from Allergists, Dermatologists, General Practitioners, Pediatricians, etc., were not routinely reconciled by their doctors. Some also reported using over-the-counter steroid creams or topical medications from family members that were never reconciled by their doctors. Members also report that follow-up information on number of finger tip units, areas of use, uses per day, days per month, etc., was not requested by their doctors. They did not feel their doctor knew which areas, how much, how often, or what type of topical medication they actually used during a given time frame. It is important for the physician to understand their patient’s pattern of use to properly evaluate the risk of developing TSWS.
Our members also feel that steroids should not be a first line treatment for eczema or dermatitis – especially for children and infants. Many feel that if they had been patch tested for contact dermatitis as a first step, they may have been more able to avoid triggers, thereby minimizing or completely avoiding use of topical steroids from the beginning.
Citations:
- “A systematic review of topical corticosteroid withdrawal (“steroid addiction”) in patients with atopic dermatitis and other dermatoses,” The National Eczema Association Task Force: Tamar Hajar MD, Yael A. Leshem MD, Jon Hanifin MD, Susan T. Nedorost MD, Peter Lio MD, Amy S. Paller MD, Julie Block BA, Eric L. Simpson MD, Journal of the American Academy of Dermatology, 2015 March, 72(3), pp. 541-549. DOI: http://dx.doi.org/10.1016/j.jaad.2014.11.024
- “Topical Steroid Addiction in Atopic Dermatitis,” Mototsugu Fukaya MD, et al. Drug, Healthcare and Patient Safety, 2014;6: pp.131–138. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4207549/
- “Corticosteroid Addiction and Withdrawal in the Atopic: The Red Burning Skin Syndrome” Marvin J. Rapaport, MD and Mark Lebwohl, MD. Clinics in Dermatology, May–June 2003, Volume 21, Issue 3, pp. 201–214 http://www.sciencedirect.com/science/article/pii/S0738081X02003656
- “Steroid Addiction.”Albert M. Kligman, M.D., Ph.D. and Peter J. Frosch, M.D. International Journal of Dermatology, Jan-Feb 1979,Vol 18, pp 23-31. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-4362.1979.tb01905.x/abstract
- “Topical corticosteroid addiction may be to blame when ‘rash’ defies treatment,” Paula Moyer, Dermatology Times, 1 October 2012. http://dermatologytimes.modernmedicine.com/dermatology-times/news/modernmedicine/modern-medicine-news/topical-corticosteroid-addiction-may-be-b?page=full
- “Topical corticosteroid-induced rosacea-like dermatitis: A clinical study of 110 cases,” Sanjay K Rathi MD and Leishiwon Kumrah MD, Indian Journal of Dermatology, Venereology, and Leprology, 2011,Volume 77, Issue 1, pp 42-46. http://www.ijdvl.com/text.asp?2011/77/1/42/74974
- “Addressing the Challenge of Topical Steroid Withdrawal,” Peter Lio MD, Practical Dermatology, September 2015, pp 41-42. http://practicaldermatology.com/2015/09/the-challenges-of-topical-steroid-withdrawalogy/
- “Facing up to withdrawal from topical steroids,” Mary C. Smith, RN, MSN; Susan Nedorost, MD; and Brandie Tackett, MD, Nursing, September 2007, vol 37, issue 9, pp 60-61. http://journals.lww.com/nursing/Citation/2007/09000/Facing_up_to_withdrawal_from_topical_steroids.46.aspx
- “Topical corticosteroid addiction and withdrawal – An overview for GPs,” Belinda Sheary, Australian Family Physician, June 2016, vol 45, No. 6, Pages 386-388. http://www.racgp.org.au/afp/2016/june/topical-corticosteroid-addiction-and-withdrawal–-an-overview-for-gps/
- National Eczema Association Education Announcement: Use of Topical Corticosteroids for Eczema. https://nationaleczema.org/education-announcement-topical-corticosteroids-eczema/
- “Steroid-Induced Rosacea-like Dermatitis: Case Report and Review of the Literature,” Amy Y-Y Chen, MD; Matthew J. Zirwas, MD, Cutis, April 2009, Volume 83, pp 198-204. https://www.ncbi.nlm.nih.gov/pubmed/19445310
- “A rosacea-like eruption of children.” JA Savin, S Alexander, R Marks, British Journal of Dermatology, November 1972, Volume 87, Issue 5, pages 425–429. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2133.1972.tb01589.x/abstract
- “Steroid rosacea in children,” HL Franco, WL Weston, Pediatrics, July 1979, Volume 64, Issue 1, pages 36-38. http://pediatrics.aappublications.org/content/pediatrics/64/1/36.full.pdf
- “Steroid rosacea in prepubertal Children,” WL Weston, JG Morelli, Journal of the American Medical Association Pediatrics (Formerly Archives of Pediatric and Adolescent Medicine), January 2000, Volume 154, Number 1, pages 62-64. http://archpedi.jamanetwork.com/article.aspx?articleid=348509
- “A prospective study of atopic dermatitis managed without topical corticosteroids for a 6-month period,” Fukaya et al, Clinical, Cosmetic and Investigational Dermatology, July 2016, Volume 9, Pages 151—158 https://www.dovepress.com/a-prospective-study-of-atopic-dermatitis-managed-without-topical-corti-peer-reviewed-fulltext-article-CCID
- Rosemarie Curley. “A systematic review of topical steroid withdrawal in children diagnosed with eczema.” PROSPERO 2015:CRD42015019001 Available from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015019001
- “Prevalence of atopic diseases and the use of topical corticosteroids. Is there any connection?” Alexander N. Pampura, Medical Hypotheses, 2005;64(3):575-8. http://www.ncbi.nlm.nih.gov/pubmed/15617870